An analysis of research both national and local, across Southend Essex & Thurrock (SET), Confidential enquiry into premature deaths of people with learning disabilities (CIPOLD) and the LD Mortality Programme Learning from Death Review (LeDeR) Programme have shown that people with Learning Disability experience a range of health inequalities, leading to higher rates of hospital admission and longer stays, worse health outcomes and earlier deaths.
Locally acute Trusts recognise that admissions for a key cohort of people with Learning Disabilities are longer or have poorer outcomes when there is no familiar person to support them.
Whilst the Hospital uses a LD Hospital passport that contains information about an individual’s clinical requirements, chronic health history, preferences, contacts etc. this cannot substitute a familiar carer being able to support patients navigating healthcare
Currently there is no clear agreement on when or if Social Care provided by the individual’s local authority or Continuing Health Care (CHC) providers funded by the Integrated Care Board (ICB) should support people on admission to hospital. Often the Hospital has to arrange ad hoc support from bank staff and is often made in crisis.
The aim of this paper is to identify how social care, providers, acute hospitals and specialist LD health services can work together to support good outcomes for people with LD in acute settings.
Support in Hospital
When in hospital people with Learning Disabilities continue to require their social care package they receive in the community, however this is often difficult to provide in an acute healthcare setting and this may exacerbate behaviours and cause difficulty in delivering healthcare or lead to worse outcomes for the adult.
Upon admission, the delivery of healthcare is clearly the responsibility of the acute hospitals, but there are certain needs which require the presence of a familiar and consistent carer, who understands the person well and who can be part of the multi-disciplinary team and where the social care or CHC provider may be best placed to meet those needs:
Behaviour support plan –often people with a positive behaviour support plan in place require a consistent approach from people familiar with its implementation; it is highly likely that the presence of these carers will improve compliance with healthcare and outcomes for the adult
Communication – where a person has limited communication and requires alternative methods to be used (sign/symbols/PECs etc), the carers most familiar with the individual’s communication style and needs enable the patient to express themselves, understand what is happening to them and, wherever possible, take part in decision making. They can also greatly assist ward staff alongside the LD Hospital Liaison Nurse, in understanding and implementing alternative methods of communication.
Autism – people with LD and/or autism may particularly struggle with the change in routine that hospital admission brings or may have sensory needs or phobias. A carer who understands this can identify where and how adaptations need to be made on the ward, can help the person adapt to new routines and comply with treatment plans.
Phobias – where people have anxieties or specific phobias around health environments, such as needle-stick, invasive procedures or other items, a person who is familiar to them can greatly alleviate their anxieties and enable procedures and tests to be carried out, often reducing time spent in hospital.
Reassurance and continuity – visiting a person in hospital and being part of discussions around care can keep the person in contact with their home environment, maintain mood and ensure that the hospital care and eventual discharge plan is familiar to social care staff and carried over into the home setting on discharge.
Outcomes
- Improved outcomes for the adult in both physical and mental wellbeing
- Shorter Stays in Hospital
- Continuity of care with a joined up and well understood discharge plan, which social care providers are in agreement, with and can implement at home.
- Reduced re-admissions
- Likely reduction in anxieties on any subsequent return to hospital the person and require less support
- Family likely to be reassured
Process
There are two cohorts:
- Those whose need for support in acute can be identified early and recorded in their hospital passport, funding arrangements agreed ahead of time and contingencies put in place should they need it. These are predominantly those with complex behaviour and phobias.
- Others will be found on admission to be more distressed or not engaging as expected despite additional hospital support and a discussion will be needed between the ward and social care. A process for quickly agreeing support and funding should already be agreed so that it can quickly and efficiently be put in place.
For both cohorts an LD risk assessment will be carried out by nursing staff on admission to identify additional needs, the type of support needed and who is best placed to meet those needs; the hospital passport will be reviewed as part of this
The assessment should reflect the person’s need (rather than available hours from a provider as needs may present differently or be met by a variety of agencies); then the local protocols should be followed to identify who is best placed to meet specific needs, considering HCA, volunteering, family or advocacy to meet needs or whether support in needed at all
See Appendices for the relevant acutes guidance documents.
Funding
The Trust is responsible for funding the clinical needs of the individual including any additional support as outlined above
Where one to one hours are available and meet the identified needs of the person, these are maintained, and a quick process is in place for Adult Social Care to cross-charge the relevant acute trust.
Where there is a requirement for additional hours identified by the hospital, the Service Placement Team will process this, and Adult Social care will cross-charge the relevant acute trust. This will be at the same rate currently commissioned be Essex County Council with the provider.
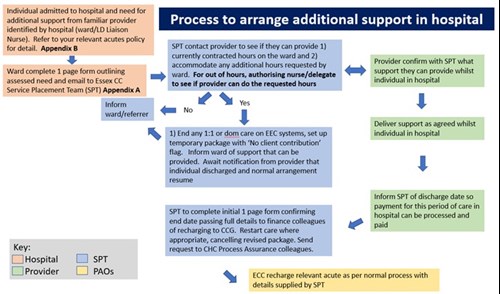
Please refer to Appendix D. For a flowchart of process and Appendix E. For 1 page In Hospital Support form
Appendix D.
Appendix E.
In Hospital Support
|
*Full Name:
Preferred name:
*Date of Birth: |
*NHS No:
Hospital No:
*Hospital name:
Mosaic No if known:
|
|
*Permanent address: |
NHS/IDT budget holder agreement (for ECC reclaiming of costs)
Name of Budget Holder:
ICB name:
Unique CCG Patient ID Code/Personal ref. (to quote on invoice):
Hours required per week:
Required Start date:
Signed:
Date: |
|
*Post code: |
Position: |
|
*Telephone No: Email contact: |
Contact No: Email contact: |
|
Name of Provider (Provider to notify SPT when normal support at home resumes):
*indicates mandatory fields, if these are not filled in, the form will NOT be processed. Please return by email SPT.PackageChanges@essex.gov.uk To ‘’Chase’’ progress phone 033301 39975 Monday to Friday or Saturday 07774337494. Please allow 3 hours for admin processing and communication with care provider. |
||||||||
|
*Staff signature: |
*Date: |
