- Experiencing memory loss, poor judgment, and confusion
- Difficulty speaking, understanding and expressing thoughts, or reading and writing
- Wandering and getting lost in a familiar neighbourhood
- Trouble handling money responsibly and paying bills
- Repeating questions
- Using unusual words to refer to familiar objects
- Taking longer to complete normal daily tasks
- Losing interest in normal daily activities or events
- Hallucinating or experiencing delusions or paranoia
- Acting impulsively
- Not caring about other people’s feelings
- Losing balance and problems with movement
What is dementia?
Dementia is one of the biggest health and social care issues of our time, with the number of people living with the condition projected to increase rapidly and no clinical treatment to prevent, slow or cure the underlying diseases it is the leading cause of death in England. Dementia is a progressive condition that can have a devastating effect, not just on the person with dementia, but also on families, carers and wider society.
Dementia is a term used to describe a range of conditions that cause a person's ability to think, remember, and reason to decline over time. It is the loss of cognitive functioning — thinking, remembering, and reasoning — to such an extent that it interferes with a person's daily life and activities.
People with intellectual and developmental disabilities can also develop dementia as they age and, in these cases, recognising their symptoms can be particularly difficult. It’s important to consider a person’s current abilities and to monitor for changes over time that could signal dementia.
You will find some helpful observation tools later on in this toolkit or take a look here
Understanding Different Types of Dementia
"As we age, it’s normal to lose some neurons in the brain. People living with dementia, however, experience far greater loss. Many neurons stop working, lose connections with other brain cells, and eventually die. At first, symptoms can be mild, but they get worse over time." (Source: National Institute on ageing)
It is important to note that Dementia is an umbrella term used to describe a range of neurological conditions affecting the brain that get worse over time.
Types of Dementia
is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. It is the most common cause of dementia among older adults.
are the result of damage to neurons in the frontal and temporal lobes of the brain. Many possible symptoms can result, including unusual behaviours, emotional problems, trouble communicating, difficulty with work, or difficulty with walking. FTD is rare and tends to occur at a younger age than other forms of dementia. Roughly 60% of people with FTD are 45 to 64 years old.
is a disease associated with abnormal deposits of a protein called alpha-synuclein in the brain. These deposits, called Lewy bodies, affect chemicals in the brain whose changes, in turn, can lead to problems with thinking, movement, behaviour, and mood. Lewy body dementia is one of the most common causes of dementia.
refers to changes to memory, thinking, and behaviour resulting from conditions that affect the blood vessels in the brain. Cognition and brain function can be significantly affected by the size, location, and number of vascular changes
Click on this link to find out more about each of these types of dementia - Understanding Different Types of Dementia.
Click on this link to find out more about each of these types of dementia Understanding Different Types of Dementia.
Delirium versus dementia
Delirium and dementia are often confused, as they are both brain disorders that cause cognitive impairment but they have different symptoms, causes, and rates of progression.
- Sudden onset of confusion and disturbed awareness
- Symptoms which can include agitation, hallucinations, and delusions
- Often caused by infections, dehydration, drug use, or withdrawal
- can be a medical emergency
- and can resolve with treatment of the underlying cause
- There is likely to be a gradual decline in memory, thinking, behaviour and personality
- Early symptoms which include memory loss, difficulty concentrating and confusion about time and place
- It is usually caused by a disease like Alzheimer's, vascular dementia, or Lewy body dementia
- It typically worsens slowly over months and years
- Can’t only be managed not resolved by treatment
What is the impact and risk of developing dementia?
There are 21,550 people aged 65 years or above who have been diagnosed with dementia in the administrative County of Essex (NHS England Digital Data). Forecast data provided by the Projecting Older People Population Information System (POPPI) anticipates that, assuming the prevalence remains constant, for Essex as a whole there will be almost 10,000 more people aged 65 and over with dementia in 10 years’ time.
It is also estimated that 15,600 working age adults are living with dementia in Greater Essex. Alongside this are those who are caring for a loved one with dementia, often over 50 hours a week.
There's no certain way to prevent all types of dementia, however there's good evidence to suggest that a healthy lifestyle can help reduce the risk of developing dementia when you're older.
That’s why it is very important that you enable the people you support to stay fit and healthy, inspiring them to take up new activities that will stimulate them both physically and mentally.
A risk factor is something that increases your likelihood of developing a condition.
Some dementia risk factors are difficult or impossible to change. These include:
- age: the older you are, the more likely you are to develop dementia. However, dementia is not a natural part of ageing
- genes: in general, genes alone are not thought to cause dementia. However, certain genetic factors are involved with some of the less common types. Dementia usually develops because of a combination of genetic and "environmental" factors, such as smoking and a lack of regular exercise
- air pollution: research suggests that air pollution may affect the brain and could increase the risk of dementia
Research suggests other risk factors may also be important. These include:
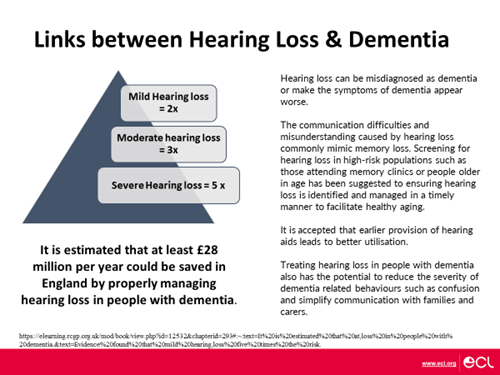
- hearing loss
- untreated depression
- loneliness or social isolation
- sitting for most of the day
Click on the image below to have a look at the 12 risk factors for dementia
This research concluded that by modifying the risk factors, around 4 in 10 cases of dementia could be prevented.
Experts also agree that what's good for your heart is also good for your brain. This means people can help reduce their risk of dementia by:
- eating a balanced diet
- maintaining a healthy weight
- exercising regularly
- keeping alcohol within recommended limits
- stopping smoking
- keeping blood pressure at a healthy level
Source - Can dementia be prevented - NHS
‘’What do you think you could do, to help lower the risk of any of the people you support, developing dementia?’’
Early onset Dementia, also known as young-onset dementia
People whose symptoms start when they are under the age of 65 are often known as ‘younger people with dementia’ or as having young-onset dementia. This is not for a biological reason but is based on the fact that 65 was the usual age of retirement for many people, historically.
There are important differences in how dementia affects younger people.
These include the following:
- A wider range of diseases cause young-onset dementia.
- A younger person is much more likely to have a rarer form of dementia.
- Younger people with dementia are less likely to have memory loss as one of their first symptoms.
- Young-onset dementia is more likely to cause problems with movement, walking, co-ordination or balance.
- Young-onset dementia is more likely to be inherited (passed on through genes) – this affects up to 10% of younger people with dementia.
- Many younger people with dementia don’t necessarily have any other serious or long-term health conditions.
Someone who is diagnosed under the age of 65 needs to adjust to living with a long-term condition as a younger person. They might be concerned about the effects this will have on their family, relationships, finances and daily life.
Find out more about this here
Dementia and Down Syndrome
People with Down syndrome have a higher risk of developing dementia, particularly Alzheimer's disease, as they age. This is because they are born with an extra copy of chromosome 21, which carries a gene that produces amyloid precursor protein (APP). Excess APP leads to the buildup of beta-amyloid plaques in the brain, a hallmark of Alzheimer's disease.
Research suggests that people with Down’s syndrome may exhibit changes in personality and behaviour in the early stages of Alzheimer’s disease before memory loss becomes evident. Often, it is small changes in routine and the person’s usual activities of daily life that indicate the possible onset of Alzheimer’s disease. Alzheimer’s disease in people with Down’s syndrome may be associated with the onset of seizures for the first time in that person’s life.
The time course of Alzheimer’s disease in people with Down’s syndrome has been reported to be more rapid than in the general population. Whether this is the case or not is uncertain as it may be a manifestation of the difficulties and delay in making an early diagnosis. By the time the diagnosis is made the dementia may already be advanced.
Source - Ageing and Dementia - Downs Syndrome Association
Down Syndrome and Alzheimers-Disease - further information and help available
What are the symptoms of dementia in someone with a learning disability?
Knowing which symptoms to be aware, of can help the person get the appropriate assessments as early as possible. There are early signs you can look out for, including:
- changes in their daily living skills
- differences in the way they approach daily tasks
- changes to their memory, reasoning or language.
As you are likely to see the person day to day, you are best placed to notice and recognise subtle changes. This could include changes in their mood or the time it takes them to carry out certain tasks. Any changes that you, or the person’s other carers, family or friends notice, can play an important part in helping to spot the early signs of dementia.
If you notice ongoing changes rather than a one-off, tell the GP or specialist learning disability team as soon as possible. They can arrange for the person to have an assessment designed to identify dementia in people with learning disabilities.
These changes can all be caused by other conditions, so it doesn’t necessarily mean that the person you care for has dementia. However, all changes should be investigated by the GP or learning disability team. Think about their personality, their likes and dislikes, as well as their current and past interests and needs.
With the right support, the person you care for may be able to continue with their daily routines, activities and hobbies for some time.
Multiple Health Conditions, Dementia and ageing
As people age, it's common for them to develop multiple co-existing health conditions, in addition to any diagnosed disability. When someone has dementia, managing these multiple conditions can become more complex and challenging.
Common additional conditions with dementia include a variety of physical and mental health conditions. Here are some of the most frequently observed:
Conditions like hypertension, coronary heart disease, and stroke are common among people with dementia.
This metabolic disorder is often seen in individuals with dementia and can complicate the management of both conditions.
Mental health issues such as depression and anxiety frequently co-occur with dementia, affecting the overall well-being of patients.
There is a notable overlap between dementia and Parkinson’s disease, particularly in older adults.
Conditions like chronic obstructive pulmonary disease (COPD) are also common in dementia patients.
This condition can exacerbate mobility issues and pain management challenges in those with dementia.
Recurrent infections, such as urinary tract infections, are more prevalent in individuals with dementia.
Understanding and managing these multiple co-existing health conditions is crucial for improving the overall health and well-being of individuals with dementia.
People with disabilities are already likely to have more than one health condition, maybe for all of their life but certainly even more likely as they age. Add in a diagnosis of dementia and you’ll realise that the management of multiple co-existing health conditions for the people that you support, requires a comprehensive and coordinated approach.
Here are some suggested strategies that you and your staff teams could consider using:
Frequent health check-ups are essential to monitor the progression of both dementia and co-exisiting health conditions. This helps in early detection and timely intervention. Enable the people you support to request an annual health check, irrespective of whether they have a learning disability or not.
Develop individualised care plans that address the specific health needs of each person. These plans should consider the patient's overall health, preferences, and the severity of their conditions. For someone with a Learning Disability, the health action plan is a good resource to use, following the annual health check meeting with the Doctor. Those without a learning disability may want to consider adapting this resource to suit their own purposes.
Ensure that medications for co-existing health conditions are managed carefully to avoid interactions and side effects. Simplifying medication regimens and using pill organisers can help.
Involve a team of healthcare professionals, including doctors, nurses, physiotherapists, and social workers, to provide holistic care. This team approach ensures that all aspects of the patient's health are addressed. For those with a learning disability, consider enlisting help from Essex Learning Disability Partnership.
Provide ongoing education and training for care staff on managing co-existing health conditions in dementia patients. This includes understanding the symptoms, treatment options, and best practices for care.
Address mental health issues such as depression and anxiety, which are common in dementia patients. Providing emotional support and counselling can improve their quality of life.
Encourage a healthy lifestyle, including a balanced diet, regular physical activity, and social engagement. These can help manage co-morbid conditions and improve overall well-being.
For those people you support who are unable to say or indicate when things are changing, your staff team’s abilities to monitor, notice and record subtle change and seek professional advice, will be key in ensuring the physical and mental well-being of people with dementia and co-existing health conditions, ultimately improving their quality of life.
Further information produced by ECC can be found here - Dementia | Provider Hub | Essex
For those people you support who are unable to say or indicate when things are changing, your staff team’s abilities to monitor, notice and record subtle change and seek professional advice, will be key in ensuring the physical and mental well-being of people with dementia and co-morbidities, ultimately improving their quality of life.
Further information produced by ECC can be found here - Dementia | Provider Hub | Essex
Southend, Essex and Thurrock Dementia Strategy.
"This strategy brings together organisations from across Health and Social Care and the Voluntary Sector to speak with one voice on our aspirations for making Southend, Essex and Thurrock places where people can live well with dementia.
The impact on all those who live with dementia, including friends, family and carers, is clear to all. It is critical that we have a strategy that looks at every element, from the very tough nettle of prevention, through early diagnosis into care, support for carers and provision of accommodation.
This updated strategy for Southend, Essex and Thurrock builds on successes and lessons of the past and will be invaluable as we work together in collaboration.’’
Cllr John Spence, Cabinet Member for Adult Social Care & Health, Essex County Council.
Following consultation with residents in Thurrock and across Southend and Essex, the Dementia Strategy ensures an approach which considers not only the provision of services, but the concerns of those in local communities who are currently facing or aware of the challenges of living with dementia. The strategy seeks to build on community assets and drive development of a high-quality dementia support offer for residents. In doing so, the Dementia Strategy provides an overarching ambition and nine priority areas for delivery through local partnerships and place-based plans focusing on local delivery and place-based action.
- Those who experience dementia, and their families and carers feel they are understood and can access the support they need when they need it
- That communities and local organisations are aware of the impact dementia has on those who experience it and their families and carers
- That support for people with dementia and their families and carers is underpinned by levels of training and expertise among professionals and volunteers
- And to further promote and enhance the conditions which will contribute to a reduction in prevalence and promoting health improvement in the long-term, recognising health inequalities and the wider determinants of health to promote better health
- Prevention
- Supporting unpaid carers
- Reducing the risk of crisis
- A knowledgeable and skilled work force
- Finding information and advice
- Diagnosis and support
- Living well with dementia in the community
- Living well in the long-term End of life
Have a look at the full document here and specifically the ‘strategy on a page’ on page 3, for more details about how the priorities have been/will be actioned.
‘What does living well mean to people with dementia?’
Information taken from International Journal of Geriatric Psychiatry | Wiley Online Library
A focus on enabling people to live well needs to consider the way in which people with dementia and carers themselves define and understand living well. Living well will mean different things to different people and expectations will relate to individual circumstances.
For example, what is required to enable someone to live well in the early stages of dementia may be very different in the later stages.
People with dementia, particularly in the early stages, have articulated what it means to live well and tend to have very individualised definitions. These to some extent relate to how they lived their lives before developing dementia and a desire to continue this lifestyle.
Get help and support
- are unsure where to start with getting dementia support
- have any concerns relating to dementia
- are looking after someone living with dementia
- are living with dementia and need support
Contact the Dementia Support Line.
The Essex Fire and Rescue Service offers free home safety visits. They will visit to assess the safety of your home and make suggestions for changes you could make.
The following organisations can help you to understand the support available and signpost you to local groups and services:
Dementia affects everyone differently, the Essex Community Dementia Support Services delivered by the Alzheimer's Society, tailor support to a person’s individual needs.
Inclusive Dementia Communities Programme
The Inclusive Dementia Communities (IDC) programme is designed to complement the Essex dementia strategy. The programme and accreditation scheme is an ECC initiative in partnership with the Alzheimer’s Society and provides a free service to Essex organisations.
Inclusive Dementia Communities in Essex have a critical role in supporting the delivery of the mission and commitments to people in Essex articulated in the Southend, Essex & Thurrock Dementia Strategy
The aims of the Inclusive Dementia Communities programme & networks include:
- Building resilience, knowledge and awareness, supporting local people and communities aiming to:
- Strengthening the response of the entire community to dementia by developing the communities’ understanding of dementia and equipping communities with the skills to support people living with and affected by dementia in their community.
- Enabling local communities, businesses and services to be inclusive of people living with and affected by dementia by:
-
- building partnerships and activity in communities
- involving and supporting people to remain physically active and engaged in their local community.
- empowering people to make decisions and live independent lives for as long as possible.
- co-delivering, enabling people to live their lives to the fullest in their local community.
Inclusive Dementia Communities Accreditation - Accreditation of local organisations through the Inclusive Dementia Communities programme will be undertaken through a recognition scheme that is proportionate to the size of organisation, service, community or business. Criteria for assessment have been developed in conjunction with people living with dementia. Submission of an aspirational statement or action plan (determined by organisation size) will be reviewed and assessed against the criteria by people living with/affected by dementia and the Inclusive Dementia Community Network. People living with/affected by dementia also undertake site visits and conduct interviews with organisations.
Workforce Training & standards - Dementia
The Dementia Training Standards Framework (DTSF) https://www.hee.nhs.uk/our-work/dementia-awareness/core-skills is an useful resource which details the essential skills and knowledge necessary across the health and social care spectrum.
A recent update and review included a number of additions regarding food, drink and oral health. The Framework is aligned to Health Education England Tiers 1-3 Dementia | NHS England | Workforce, training and education (hee.nhs.uk) while Skills for Health do not provide resources for Tier 3 training the learning outcomes are included and equivalent training is available and should be included in CPD.
Note the Government intention for proposals to reform the Adult Social Care Workforce Pathway over future years. https://www.gov.uk/government/publications/care-workforce-pathway-for-adult-social-care.
Dementia and completely listening to the workforce
Charles Bonnet syndrome also effects those with sight loss and can often be misdiagnosed as dementia when people describe the hallucinations they see.
What will you do differently, to help the people you support, who are diagnosed with Dementia, to age well?
“What actions do you need to take now, to ensure that your staff teams understand the impact of falls and dementia on someone who is ageing with a disability?”
Apps for use at health appointments

Live Transcribe – provides free real time speech to text transcription making conversations with health professionals more accessible for those who are deaf or hard of hearing - Live Transcribe - Caption speech in real time.

Relay UK – helping people with hearing or speech difficulties communicate over the phone using a national relay service. Register to be able to use the function with emergency services. Relay UK - homepage | Relay UK

Signvideo – BSL 111 service open 24 hours a day NHS 111 - SignVideo : SignVideo

Seeing AI – can read documents out loud for patients – useful if asked to sign a document to ensure you know what is being agreed to. Also assists with daily tasks by describing photos and identifying people and products. Seeing AI - Talking Camera for the Blind

